Madagascar: first open-heart surgery

The Franco-Malagasy medical team has been busy working on 8-year-old Finoana for the past three hours. In this brand-new operating theatre, entirely refurbished thanks to skills sponsorship by Bouygues Bâtiments International and equipped with state-of-the-art equipment, the faces are concentrated. The atmosphere is calm, the instructions clear and the gestures extremely precise. Each of the 19 people working on the technical platform – nurses, anaesthetists, cardio-paediatricians, surgeons – go about their respective tasks. The extracorporeal circulation machine that takes over from the heart for the duration of the operation is running at full speed. You can barely hear the exchanges between the French volunteer carers and their Madagascan counterparts, who are in the midst of their practical training.
Marielle, the country’s first child to undergo open-heart surgery
Behind the OR door, in the intensive care unit, 13-year-old Mariella from Fianarantsoa (south-central France) sits upright in her medical chair. Still connected to a multitude of machines, the young girl beams. Three days ago, she underwent IVC (Interventricular Communication) surgery, making her the very first Malagasy to have undergone open-heart surgery in her country. ” Just before the operation, I was very, very scared,” she articulates painfully, “but I told myself I had to be brave, because I had to face this ordeal anyway if I wanted to live.” Her features drawn but her eyes sparkling, she confides in a whisper: “I feel like my life has changed. I feel like I’ll be able to do anything now.”


Sitting, standing. Sitting, standing. Rolland and Alianjarasoa, Finoana’s parents, can’t stand still. Their child has been in the hands of the doctors for six hours. In the small hospital room made available to the families, the parents of the three other children who have already undergone surgery try to relax them by talking about the weather, which is very cool at the start of this austral winter. For this pastoral couple from the suburbs of Antananarivo, their son’s operation in Madagascar is a blessing. “From his sixth week of life, the doctors knew that Finoana had something abnormal. After a series of tests, a heart murmur was detected. Soon enough, we knew we had to operate,” recalls his mother. ” When we were told last month that Finoana had been selected to undergo the first open-heart surgery in Madagascar, we didn’t hesitate. He had been waiting to go abroad for over four years. Covid had blocked everything”.continues his dad.

Suddenly, there’s a knock on the door. The parents freeze. Dr Pierre Maminirina, thoracic and cardiovascular surgeon at Nantes University Hospital and volunteer doctor for La Chaîne de l’Espoir, enters the room with his team. ” The operation went well,” announces the man who operated on their child, in Malagasy. Alianjarasoa and Rolland stifle a sob of relief.
Born in Madagascar, Dr Pierre Maminirina grew up and studied medicine on the Big Island. So, “operating here, on the spot”, he explains, “is a bit like doing a service for the children of my country”.
Training, the key to empowerment
Training” is a fundamental part of the program. The presence of the Malagasy-speaking doctor on this mission is a great advantage for both the French and Malagasy teams: exchanges are facilitated by the use of both languages. The 13 volunteers accompanying the surgeon take real training time, to pass on as much information as possible to their Madagascan team-mates, while allowing them to intervene according to their degree of competence.
For Finoana’s operation, surgeon Lucas Randimbinirina assisted the French volunteer. Opening the thorax, fitting aortic cannulas, etc. the young surgeon from Cenhosoa, recently returned from a training mission in Dakar and La Réunion, dexterously performed the surgical gestures dictated by his mentor.

“Setting up a local team that shares the same objective as La Chaîne de l’Espoir – to bring care to children suffering from congenital heart disease in Madagascar – is my greatest source of pride.says Dr Pierre Maminirina, with a gentle touch.
A wish that the surgeon has often expressed in the past. “At the CHU in Nantes, I often operated on little Madagascans who had been taken in by La Chaîne de l’Espoir. Each time, I said to myself what a shame it was that there were no facilities to treat them in their own country. The advantage of this project is that we won’t have to send them abroad. We’ll be able to treat them here. And the fact that they can stay with their families is very important for their morale and their recovery. “
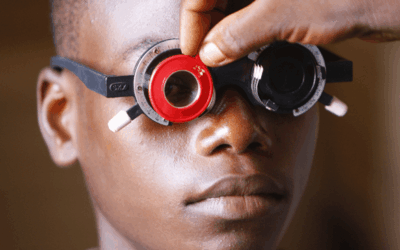
The importance of screening

This long-term project is perhaps best embodied by Dr Jean-Bernard Selly, cardio-pediatrician at the CHU de La Réunion, and Dr Dany Ravaoavy, cardio-pediatrician at Cenhosoa. Every Friday afternoon for the past four years, Dr. Dany has been seeing children with complex heart disease in his office. At 2 p.m. sharp, he logs on and enters into a tele-expertise with a medical-surgical team based in La Réunion (a surgeon, an anesthetist and a cardio-pediatrician). Objective: to determine whether the child requires urgent care and evacuation.
But for these little patients from the four corners of the island to find their way into Dr. Dany’s office, a real revolution in the way screening is carried out first had to take place. La Chaîne de l’Espoir has been mobilizing since 2018, thanks in particular to the support of Agence Française de Développement (AFD). As part of this effort, Dr. Dany regularly travels the provinces to train practitioners in direct contact with children. Whether medical staff, paramedics, community workers or nuns, they learn to recognize the clinical signs of heart disease. The aim is to help families make the right diagnosis.
“There is a real positive outcome. Here in Tana, we receive younger and younger children, sometimes infants, who have been sent to us by colleagues in the bush. This is the case of the four children we have operated on. Their malformations were systematically detected by local practitioners, referents whom we had trained,” says Dr Dany with satisfaction. “What we have achieved together this week is historic for the country”, he says.he testifies.
If the Cenhosoa has become a cutting-edge diagnostic center, it’s also because its staff have built up a wealth of expertise, acquired through training missions abroad.
Dr Dany travels several times a year to the University Hospital of La Réunion to continue his collaboration with Dr Jean-Bernard Selly.
“When we started the project with Dany, we were seeing a lot of children whose pathology had been detected too late,” explains the head of the congenital and pediatric cardiology department at the CHU de La Réunion. “They were ‘outdated’, i.e. the timing for surgery had expired. Their life expectancy was greatly reduced. However, as Dany became more and more efficient and his network grew, the change was real: patients were taken into care early.”
Detecting a child so that he or she can be operated on in the allotted time is a major challenge. “The truth is that, on a regular basis, children cannot be sent abroad in time and die. Having a center here in Madagascar that performs open-heart surgery offers real hope. continues the French doctor. Obviously, to start with, it will be the simplest cases that will be taken on. But if the program continues to make good progress, within five to ten years, the children for whom Dany and La Chaîne de l’Espoir fight every week to find an organization to finance their evacuation to Reunion or mainland France, will no longer have to look for somewhere else to go. They will be operated on here. There will be fewer transfers. Fewer deaths, too.
Hygiene at the heart of young patient safety
As you pass through the doors of the operating theatre, intensive care and sterilization rooms, you enter a whole new world. It’s as if you’ve suddenly moved to another country. Here, everything stands out from the rest of the hospital. From the bright white walls to the state-of-the-art medical equipment, from the cleanliness of the floors to the simple bins for sorting used equipment. “ We had to adapt to the constraints and revolutionize the hospital,” comments Sandrine Linares, hygienic pharmacist, facetiously. For, as the volunteer doctors remind us, “these operations were carried out under the same conditions of quality, safety and hygiene as if they had been carried out on Reunion Island or in mainland France.”


Power cuts, water supply, blood tests, treatment of medical fluids, sterilization of surgical equipment: solutions had to be found to tame the many realities of Malagasy daily life. “The success of heart surgery is not just a matter for the surgeon. It’s much broader than that. It’s the anesthetists, perfusionists, cardiopediatricians, resuscitators, nurses… but also all the people responsible for hygiene and housekeeping. Behind-the-scenes operatives who do work that isn’t necessarily rewarding, but is absolutely essential if the medical team is to work properly”, Sandrine Linares reminds us.
So, here too, staff training in hospital hygiene was a major pillar of the mission. Demonstrating appropriate techniques, training in the use of cleaning products and specific equipment, teaching the basics of contamination: everything was broken down to be properly integrated, and new procedures were created to prevent and control infections.
“You can’t clean an operating theatre or intensive care unit the same way you clean your own home. There are many parameters to control, gestures, frequencies and specific cleaning techniques to adopt. And the staff were fantastic. They all immediately understood the magnitude of their task, and were keen to change the way they operated,” says the hygienist-pharmacist.
A new life for Finoana

Back to the intensive care unit. Finoana opens her eyes, observes the machines beeping, the incessant ballet of nurses, radiologists and physiotherapists. Vazahas” (foreigners) but also Malagasy. The child was operated on less than 24 hours ago. His parents should be arriving at any moment. He smiles peacefully. His speech slow and weak, he murmurs: “I can’t wait to play soccer again with my little brother and sister. I’m glad I had the operation, and especially glad I wasn’t sent abroad. I was afraid of that option, because I knew it meant I’d have to go off on my own without my mom and dad,” he says. “Thank you to the doctors for coming here, thank you to them for choosing to operate on me.”
Discover our global action to improve access to surgical care for children throughout the Indian Ocean.