Cambodia: from training to empowerment
“It all started in Cambodia. “

When Dr. Gérard Babatasi, Head of Cardiac Surgery at the Centre Hospitalier Universitaire (CHU) Caen Normandie and Vice-Chairman of La Chaîne de l’Espoir, recounts twenty-five years of action in the country, the entire history of the association comes into focus. ” It was here that we launched our missions in 1998, performing the country’s first open-heart surgery.
We launched our first construction and equipment project there, with the inauguration of the Phnom Penh Cardiology Center (PCCC) within the Calmette Hospital in 2001 and the training of staff. We then opened the Children’s Pavilion in 2003. “
From one support to another
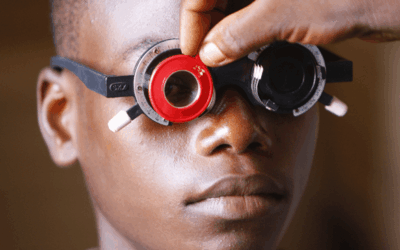
The success of these initiatives underlines the association’s intervention philosophy: trained by La Chaîne de l’Espoir’s medical teams, staff at the Calmette hospital now perform heart surgery on adults and adolescents on their own. The program to support training and access to care was completed at the end of 2022. Today, our support for Cambodia continues to expand, with training support for Kantha Bopha Foundation teams at two sites (Phnom Penh and Siem Reap, in the north of the country), in cardiac, orthopedic and neurosurgery.
Following the opening of cardiopediatric units in Kantha Bopha hospitals by La Chaîne de l’Espoir teams in Siem Reap in 2011, and in Phnom Penh in 2019, La Chaîne de l’Espoir’s volunteer healthcare professionals have carried out two missions a year to train their Cambodian colleagues. Here, too, the staff are now largely autonomous, and support will continue with a single annual mission to assess and upgrade their skills.
“ In particular, there is a need for the management of open-heart surgery on infants, as well as rheumatic valvulopathy. This requires specialized expertise and equipment “explains Dr Gérard Babatasi.
Orthopaedic and neurosurgical training
In neurosurgery, too, training initiatives are bearing fruit: senior local neurosurgeons have acquired the skills to handle the most common cases, and training is now focusing on new recruits and onanesthesia in pediatric intensive care.
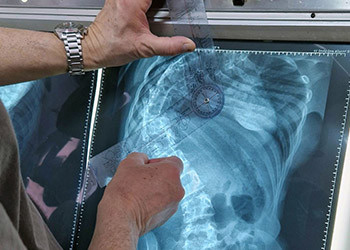
For orthopedic surgery, two missions are organized per year. These are aimed at more complex cases, such as scoliosis.
The continuation of regular missions will enable local orthopedic teams to become self-sufficient within four or five years.